This past October, several members of the Cantina team attended and spoke at the Connected Health Conference here in Boston. It was truly a privilege to collaborate with healthcare leaders, providers, and innovators. Together, we learned about balancing the human and technological aspects of connected health to create the best possible outcomes for patients. As we spoke to conference-goers, we uncovered three main themes: interoperability, greater access to care, and value-based care. These themes closely relate to consumer health & wellness, condition management, and data science. We anticipate these themes will drive healthcare innovation for years to come.
Interoperability and Data Integration
The Healthcare Information and Management Systems Society (HIMSS definition of interoperability is “…the ability of different information technology systems and software applications to communicate, exchange data, and use the information that has been exchanged.” Interoperability improves patient outcomes and reduces care gaps by providing improved access to patient data. This benefits both the providers and patients. Patients benefit from access to a greater variety of care management tools. According to a study by the Airedale NHS Foundation Trust, simply creating a bridge between at-home care and provider care with telemedicine reduced hospital admissions by 35%. Patients are also more likely to follow wellness management recommendations and chronic condition management routines, because they have more power to choose how to manage their condition.
When providers have access to patient data and medical records, it’s easier to build connections across platforms and to keep a holistic view of a patient’s health. A recent HIMSS report shows 79% of respondents agreed they would like to have more data about patients between visits. Data-sharing and integration is so key, the Dana-Farber Cancer Institute and the Biden Cancer Initiative are recruiting more than 100,000 cancer patients from the U.S. and Canada to share their medical records so biomedical researchers can use the data to drive innovation in cancer research.
While proprietary digital tools can help bridge this gap, the best way to ensure everyone in a patient’s care team has access to data is to distribute it with connected health products and services. This also means less time is spent manually entering information into systems, and less information is lost as patients interact with these touchpoints.
Designing for Interoperability
More often than not, UX designers are called upon to mitigate the experience gaps created by a lack of interoperability. Anyone who’s had to manually provide resume information, after already submitting a PDF to a company’s HR system, can testify how frustrating this can be. What’s an unfortunate annoyance in some industries can be catastrophically life-threatening in situations when such data fragmentation causes the loss of patient healthcare information (PHI).
There are a few methods to achieve full interoperability. Determining which method should be used is a conversation involving the full product team triumvirate—business, engineering, and design. In the healthcare space, this decision is especially critical.
Many companies strive for a consolidated data model, when they may be better served with a distributed model. Netflix’s microservices model is a great example of this. Because Netflix values speed and flexibility, it focuses on maintaining APIs between 200+ microservices instead of trying to have a single source for all data. When multiple touchpoints are created by the same company, maintaining an API with a common key means all products can be developed without fear of impacting each other. This translates to easier integrations with healthcare partners, because custom integrations don’t have to be built—access to APIs can be given to partners instead.
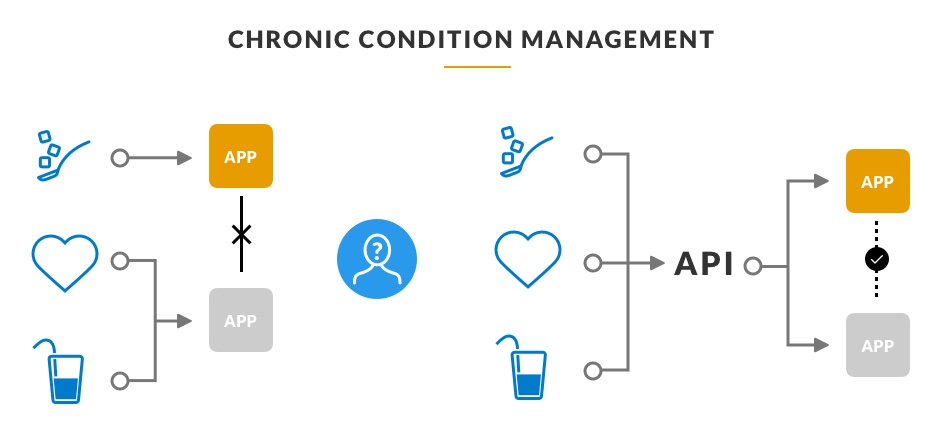
Let’s use the example of a hypothetical health tracker for someone with a chronic condition. They may be trying to deal with issues related to sugar and water intake, but the tracker is only tracking vital statistics and hydration. Another company (or a division of the same company) decides to work on a connected blood sugar tracking device, which is also available to the patient. Suddenly, this patient is managing their condition through multiple apps and devices.
Hard-coding a connection between both apps limits the ability to integrate new touchpoints down the line; however, a shared API means compatibility across existing and future touchpoints. Sharing information across touchpoints and having a complete view of their health is a clear benefit to the user. Keeping users in the driver’s seat with their data leaves them feeling more invested in their care, creating better outcomes.
Greater Access to Care
In a digital sense, increased access to care has two meanings. The more literal sense is care networks. By serving communities who may otherwise not have access to treatment or preventative medicine, digital touchpoints improve access to care for specific patient populations. Much like how opening a new surgery center or acute care facility increases access to in-person care for a segment of a city’s population, digital touchpoints expand a general practitioner or healthcare system’s footprint across a specific community. Increased access to care can also mean creating access to treatment or preventative medicine in disciplines which previously required a physical presence, regardless of proximity to the point of care.
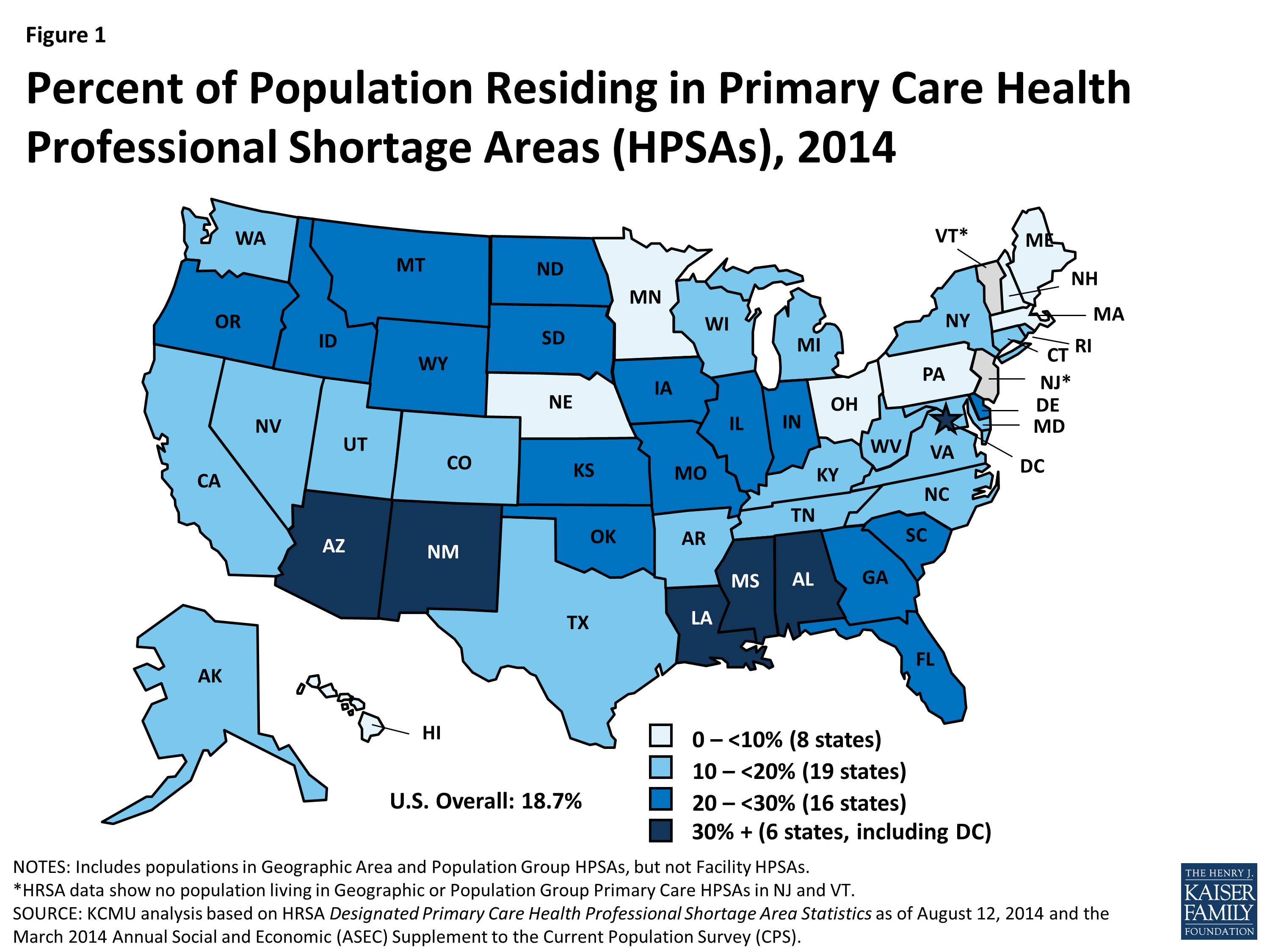
Increased access to care matters for a multitude of reasons. 25% of the US population lives in a rural area, but is serviced by only 10% of the physician population. Adding a digital touchpoint like text messaging can improve patient appointment adherence by up to 40%.
For patients in rural areas, digital care touchpoints may be their only opportunity for truly healthy lives. For patients in urban areas, having a connected health option helps fit care into their schedule in a crucial way, especially for those working multiple jobs or facing other care challenges.
Designing Greater Access to Care
A complete design process uncovers insights for innovative ways to digitally deliver healthcare solutions. Lemonaid Health is a remarkable example of this in the women’s health space. Lemonaid provides access to birth control medication through an online visit, and, through partnering with medication delivery services, a discreet alternative which also lowers the cost of care and has disrupted the traditional marketplace.
Lemonaid uses technology like video chat and webcam photos to securely identify and treat patients. Other healthcare experiences may use different methods, like administering tests using built-in phone technologies, asynchronous modes of communication, or AR/VR to get the patient and provider in the same digital room. In-home testing, through mail-in kits or good old-fashioned clinician house calls can also provide an alternative for costly healthcare facility visits
Value-based Care
Lastly, underpinning all of the changes impacting the healthcare landscape is value-based care. Creating a patient-centered healthcare experience may sound suspiciously close to creating user-centered experiences for good reason; in short, human-centered design and value-based care are inseparably entwined. Through patient surveys and quality-of-life follow-ups, value-based care holds everyone in healthcare accountable for the real results they’ve created by reimbursing based on patient outcomes, not volume. Ryan Walsh, MD, Chief Medical Information Officer at the University of Texas Health Sciences Center at Houston says, “Value-based care is here to stay… As we see more large-scale vertical integration, we’ll see employers, insurers, and governmental agencies demanding cost and quality outcomes, and at scale.”
Value-based care is here to stay… As we see more large-scale vertical integration, we’ll see employers, insurers, and governmental agencies demanding cost and quality outcomes, and at scale. Ryan Walsh MD, Chief Medical Information Office at the University of Texas Health Sciences Center
Human-centered design directly impacts value-based care because it creates a process to encourages the business to consider what user motivations are, and create business goals to match. One process for enabling this is co-design. Cantina strongly believes in co-designing with users to ensure their needs are being considered from the beginning of the design process, and works to empower all of their clients with co-design. Observing user behavior and pain points helps solve actual problems, not hypotheticals. Once a solution has been designed, tracking outcomes by setting measurable experience metrics means not guessing if touchpoints are effective.
The value of care can also be increased through digital health tracking and coaching. HIMSS recently found patients paired with a tracking coach had a 58% reduction in their risk (compared to those treated with medication at 31%). Healthcare providers are only with patients at certain care journey touchpoints. Rather than leaving patients to fend for themselves or spreading providers even thinner than they already are, digital touchpoints coach patients into being their own wellness champions. This can ultimately reduce their time spent in treatment through increasing time spent in condition management and prevention.
Designing for Valued-Based Care
NYU Langone Health recently launched a suite of digital tools to help patients. By providing patients with tools to manage their relationship with the health system, NYU Langone mitigates many of the common worries a patient has about the entire healthcare experience. Furthermore, it empowers clinicians, by giving them access to patient information in ways they didn’t before.
It would be easy to consider only the ability of a health system to provide better medical treatment. NYU Langone’s use of digital touchpoints proves they’re thinking about the entire patient experience within a broader service design. Surfacing tools to provide patients with greater control over the back-end process (like payment, waiting for an appointment, or working with insurers) can drive a higher overall quality of care. Service design in this regard allows patients to co-design their experience as it’s happening. This new co-designed system improves their quality of care, by consolidating and distributing their medical information more accurately across the healthcare system.
The Future of Connected Health and Design
Connected health requires bringing together business acumen, engineering architecture, and holistic experience strategy in ways we’ve never experienced before. Thomas Fisher from the University of Minnesota and Jess Roberts of Allina Health emphasize, “Design provides a rigorous method of reframing the conversation about ill health, re-defining the nature of the problems and re-imagining new and less conventional approaches to addressing it. In the process, design changes cultures.”
Design provides a rigorous method of reframing the conversation about ill health, re-defining the nature of the problems and re-imagining new and less conventional approaches to addressing it. In the process, design changes cultures. Thomas Fisher at the University of Minnesota and Jess Roberts of Allina Health
Interoperability, greater access to care, and value-based care can all benefit from a more strategic design approach. By applying new design methods to the business, and not designing touchpoints in isolation, it’s more likely to uncover opportunities to be inclusive in serving patient populations. Not only does this create better outcomes for users, it keeps companies competitive in a changing landscape where we have more options than ever for managing our healthcare and wellness.