Inclusivity in healthcare and digital transformation are inseparable from each other. As discussed in Part 1 of this series, attempts to innovate and modernize in healthcare bring many challenges related to inclusivity in digital health. Healthcare organizations can’t hope to change the patient experience and generate better outcomes for underserved groups without transforming the way their business functions. However, it is important to understand—when applying service design thinking—digital alone isn’t enough. Offline and online channels must be considered at every touchpoint.
Cantina advocates for designing with users. During the service design process, designers should invite patients into the room with staff. Their journey through the healthcare system needs to be empathized with and carefully considered. What was going through their minds as they used a product or service, or interacted with a healthcare provider? How did they feel? When did the system fail them? When did it support and nurture them?
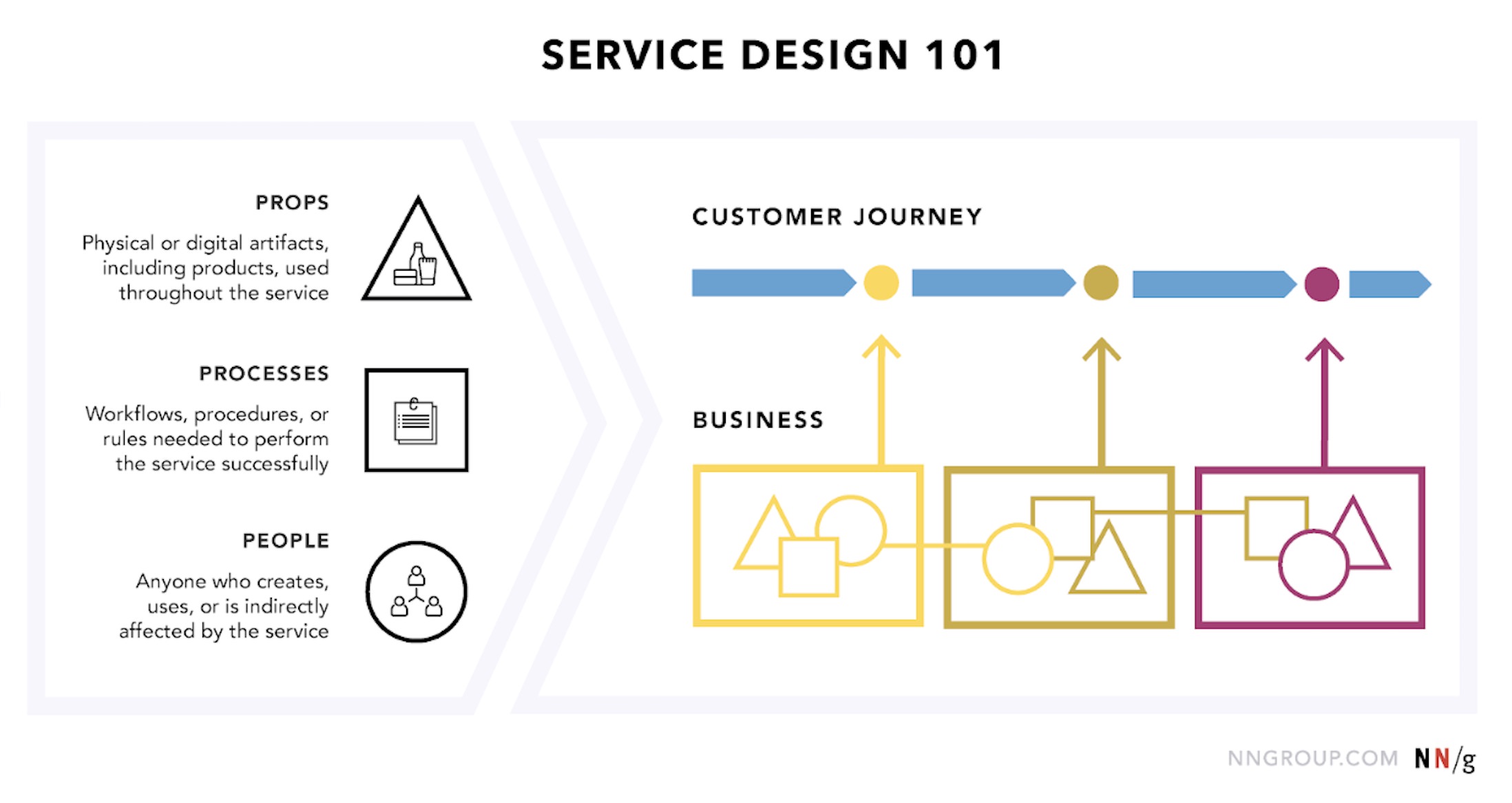
By the same token, the clinician and staff experience must be thoroughly examined. What are their pain points? Where can they be equipped with better tools to help patients? Is the organization set up to help them succeed, or does it get in the way? With service design doing, the focus is holistic. Front-end (what the patient sees and experiences), back-end (what happens behind the scenes to deliver the patient experience), support processes that make it all happen, and online and offline channels and interactions; all must inform the ultimate service design.
Service design teaches:
- Start from the customer need. Generate problem statements from these. Consider the possible problems to tackle, and which ones have the biggest impact on the patient experience.
- Create a vision around meeting customer needs. Become obsessively patient-focused when creating solutions. Design every touchpoint—those visible to patients and those that are happening behind the scenes.
- Co-design with patients, clinicians, and support staff so that services have tangible outcomes. Reshape organizations to tackle customer pain points and deliver better experiences and outcomes.
Mitigating Bias in Service Design
Designers must also acknowledge their own implicit bias during the service design process. An emerging focus across design disciplines (experiential, architectural, industrial, and more) is transcultural design: understanding that designers have limitations and assumptions when designing for those from different cultures. There are many lessons to be taken from the NPR design team’s methods of overcoming cognitive bias. Chief among them is assumption mapping. This is not just for stakeholders in business organizations. Designers can make efforts to identify their own biases up-front, based on their own personal experiences and journeys.
Inspiration can be taken from the city of Charlotte, North Carolina. By holding a summit with the community, the health systems serving Charlotte’s population were better prepared to tackle the unique challenges facing them. As a result of their Engagement Cafe, “Both the Carolinas HealthCare System and Novant Health provide educational resources on patient information access, Insurance companies provide access and online education, [and] The Charlotte Mecklenburg Library provides basic digital literacy workshops and tutoring in various issues.”
Impacting Healthcare Through Service Design
The Greensboro Health Disparities Collaborative is well-versed in service design. Through their partnership with Accountability for Cancer Care Through Undoing Racism and Equity (ACCURE), they followed patients throughout their care journey.
By identifying moments of unconscious bias, they better understood how to build care networks for the full diversity of their patient population.
The low hanging fruit is bias and inclusivity training. However, there also must be support networks for complications. Treating the whole patient means financial and emotional support for those who are struggling, like Kaiser Permanente building a network to address people’s social needs. It means helping with social problems (e.g., domestic violence or housing instability), and being persistent with following up on appointments.
Particularly in at-risk neighborhoods, access to digital tools to manage health and wellness is not a guarantee. Even if health systems are able to offer apps or wearables, they need to offer education to improve digital literacy and health literacy. Minnesota-based HealthPartners used this approach to create decision support tools and proactive care networks. As a result, they reduced the gap in colorectal cancer screening rates between Latinx and Caucasian patients.
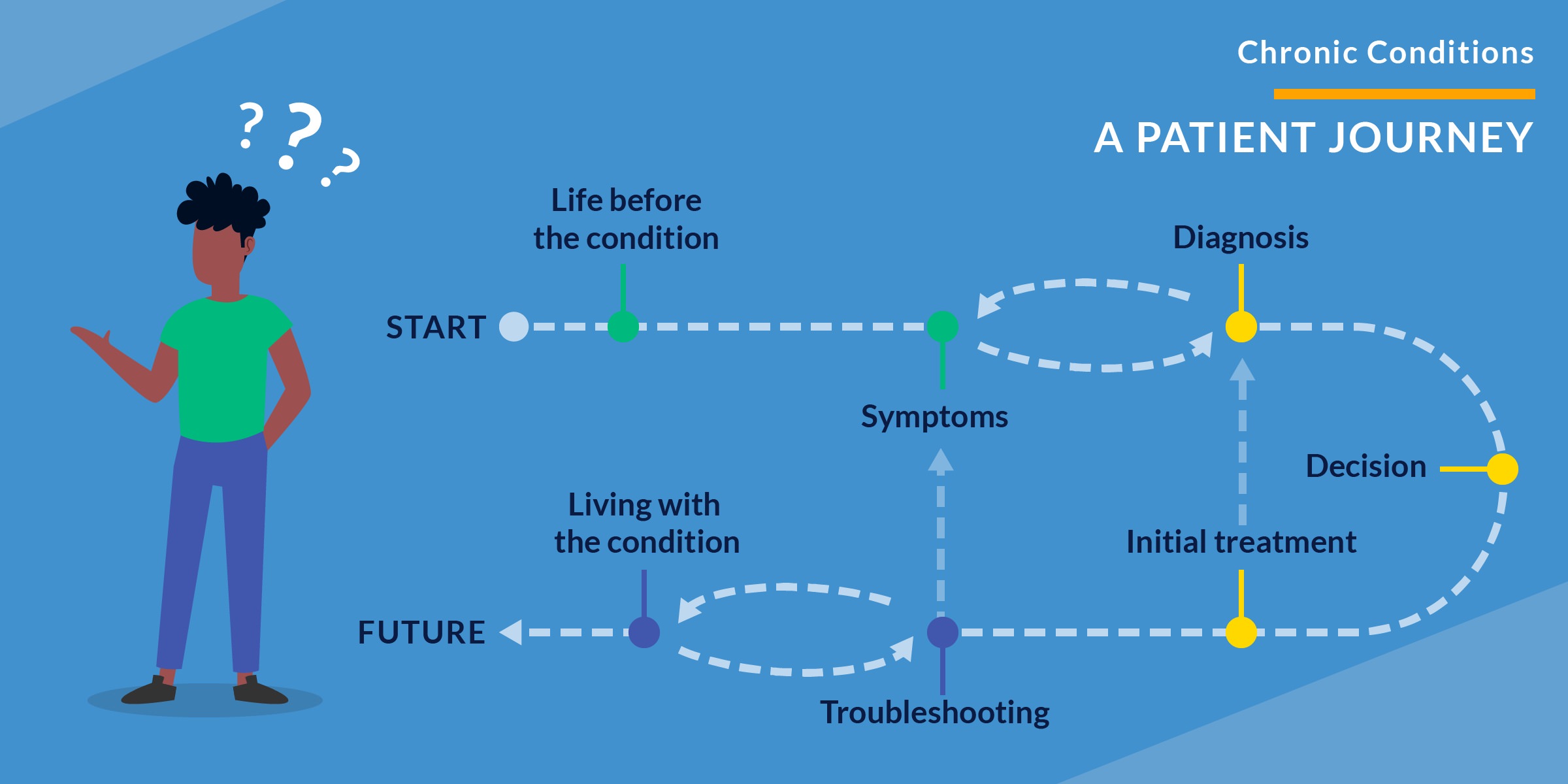
No matter the patient, a chronic condition diagnosis can be traumatic. Technology is not the solution here. Genuine human connection, empathy and concern for the patient must take center stage, with technology playing a supporting role at most. Services must be designed to follow up with patients about care options and manage their condition. Staff need training to be sensitive and inclusive when working with patients. Health systems like the Frederick (Md.) Regional Health System are leading the way with task forces and clinics devoted to ensure LGBTQ needs are met. The patient’s mental health is equally as important as their physical health. By focusing on patient-reported outcomes, chances of successful treatment are far more likely than if the focus is purely on medically-recorded outcomes.
Move Slowly and Fix Things
Many of the examples above may seem deceptively simple. Patient-reported outcomes are a no-brainer for many not in healthcare. Shouldn’t healthcare’s efficacy be largely based on what the patient is feeling and experiencing, and not on how many beds are filled or patients are seen? Why not strive to create systems, incentive models and support networks focused on delivering the best possible patient experience and outcomes for everyone?
Designers must be mindful. In healthcare, optimization and operational efficiency are valued over innovation. Keeping costs and risks low and improving patient outcomes is the name of the game. “Move fast and break things” is more tolerable when building gaming or food delivery apps. It can’t be done when designing for people’s health. It’s all well and good when a team breaks a gaming app. It’s another matter when a team breaks the telemedicine platform for pediatric surgery patients in rural Montana.
For these reasons, designers should categorize their work into “innovation portfolios”. By considering touchpoints through the lenses of incremental, adjacent, or transformative innovation, healthcare executives and decision-makers can better grasp the magnitude of the changes recommended, and plan roadmaps accordingly.

Important, too, is a healthy grasp of change management. Designers must adapt strategies for business outcomes. There are reasons why age-old business strategies have endured for so long. Top-down and grassroots methods for adoption, ownership over changes, genuine fears about changes (rational and emotional) being addressed, and leading with the culture are all needed. A surgical checklist may be all-but-guaranteed to reduce errors, but unless those using it are personally invested, adoption will prove difficult.
Designing for a Disease-Free World
Healthcare is moving from a focus on physician-reported outcomes and volume-based care to overall well-being, interoperability, and the patient experience. Preventative care and telemedicine are leading the way, but designers must think bigger.
Healthcare is full of some of the most intelligent and driven people one will meet in any profession. Many have been working for decades to keep people well. Any designer who seeks to transform healthcare would do well to remember that.
Healthcare designers must be as obsessively focused on the patient as the physicians, nurses, pharmacists, and other providers in the healthcare ecosystem. The focus must be on the front-end and back-end processes orchestrated to manage someone’s healthcare journey. Digital transformation, change management, and the crafting of touchpoints in online and offline channels—all impact the holistic patient experience. Only when these complex ecosystems are considered in their full context, centered on the people they are meant to help, will lasting success be created.
The first step in designing inclusive services is crafting an experience strategy. If you’re interested in learning how strategic design can enable digital transformation in healthcare, check out Cantina’s Experience Strategy Method Cards. If you’d like to learn more about applying service design principles and bringing experience strategy to your organization, contact us today.



